Panic symptoms in schizophrenia: Comorbidity and clinical correlates?
Short Communication
Panic symptoms in schizophrenia: Comorbidity and clinical correlates?
HALIS ULAS, MD, KOKSAL ALPTEKIN, MD, BERNA BINNUR AKDEDE, MD, MEVHIBE TUMUKLU, MD, YILDIZ AKVARDAR, MD, PHD, ARZU KITIS, MD AND SELMA POLAT, MD
Department of Psychiatry, Medical School of Dokuz Eylül University, Izmir, Turkey
Abstract
The aim of the present study was to investigate the prevalence of panic attack (PA) and panic disorder (PD) in patients with schizophrenia and detect the clinical features. Forty-nine patients with schizophrenia were included in the study. Positive and Negative Syndrome Scale (PANSS), Hamilton Depression Rating Scale (HDRS), Clinical Global Impression (CGI), Extrapyramidal Symptom Rating Scale (ESRS) and Bandelow Panic and Agoraphobia Rating Scale were administered. Fifteen patients were found to have PA and seven patients had PD. Patients with panic symptoms had higher scores of PANSS, HDRS, CGI and ESRS. Comorbid panic symptoms in schizophrenia may be related to positive symptoms, extrapyramidal side-effects and depression.
Keywords: clinical features, comorbidity, panic attacks, panic disorder, PANSS, schizophrenia.
1.Introduction
Lifetime prevalence rates for panic attack (PA) without agoraphobia (AG) have been reported to be 6.5%-22.7%, 0.85% for PA with AG without panic disorder (PD) and 0.4%-3.7% for PD without AG in the general population.1-6 Population studies examining psychosis and PA suggest that they may be commonly associated. Comorbid PA in schizophrenia was reported to be 28–63%.7–13
National Comorbidity Survey reported high rates of panic disorder among patients with non-affective psychosis. Those with non-affective psychosis were sevenfold more likely than the general population to have PD.14
It was suggested that PA was related to higher doses of antipsychotic drugs.8,9 Comorbidity of PA and PD may aggravate symptoms of schizophrenia and make the treatment more difficult.15
PA are associated with significant functional impairment, risk of psychiatric comorbidity and suicidal ideation and behavior both when they occur alone and when they co-occur with other psychiatric disorders.15-17
The aim of the present study was to investigate the prevalence of PA and PD among patients with schizophrenia and evaluate the clinical features.
2.Methods
2.1. Sample
Forty-nine patients (23 women and 26 men), who met DSM-IV criteria for schizophrenia were consecutively enrolled in the study. They were assessed with a questionnaire addressing sociodemographic and clinical characteristics. The study was approved by the ethics review committee of Medical School of Dokuz Eylül University.
2.2. Instruments
The volunteers were interviewed by a psychiatrist using the panic and substance abuse modules of Structured Clinical Interview for DSM-IV (SCID) in order to ascertain the existence of comorbid PA or PD and substance abuse.18 Positive and Negative Syndrome Scale (PANSS),19 Hamilton Depression Rating Scale (HDRS),20 Clinical Global Impression (CGI)21 and Extrapyramidal Symptom Rating Scale (ESRS)22 were administered to all individuals to measure the difference in severity of psychopathology between patients with and without PA. Bandelow Panic and Agoraphobia Rating Scale (BPARS)23 was administered to the patients with PA.
2.3. Statistical analysis
All statistics were analyzed using SPSS version 11.0 (SPSS, Chicago, IL, USA). Categorical variables were compared using X2 test, and Mann–Whitney U-test was used for continuous variables.
3.Results
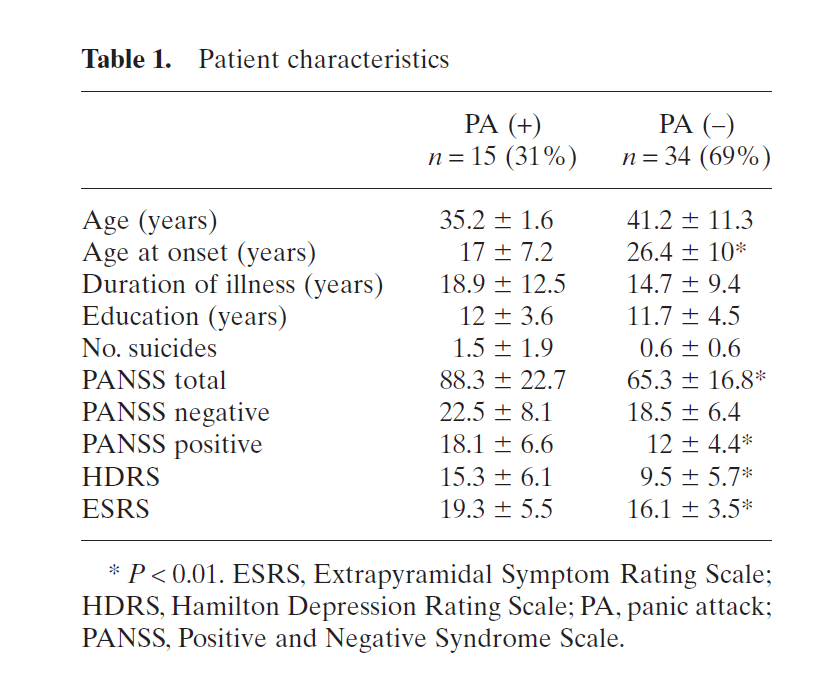
Patients had a chronic course of illness (duration of illness 16.00 ± 10.54 years). Panic symptoms of all patients were occurred after the diagnosis of schizophrenia. None of them had acute psychotic exacerbation over the last month. All patients were on antipsychotic treatment. Only two patients with PA and four patients without PA were using typical antipsychotic. All the others were on atypical agents. Fifteen patients (31%) with schizophrenia had PA and seven patients (14%) met criteria for PD. Sociodemographic and clinical characteristics of patients with and with out PA are given in Table 1.
The number of male patients with PA or PD was twofold higher than that of female patients. There was no relationship between PA and suicidality and substance abuse. Early onset patients (<18 years) had more frequent PA compared to late-onset patients (P = 0.003). No difference between typical and atypical antipsychotic was seen in relation to PA and BPARS scores.
4.Discussion
These results parallel findings of high rates of PA and PD in schizophrenia in previous studies.7–13 The present findings highlight the importance of assessing comorbid panic symptoms in patients with schizophrenia. It is known that patients with PA had significant functional impairment and more service use than patients without panic symptoms.15,17
Bayle et al. reported that there was no gender difference between patients with and without PA,6 but it has also been reported that PA was higher in female patients with schizophrenia.11,17 In the present study the number of male patients with PA or PD was twofold higher than that of female patients, which verged on being statistically significant (P = 0.056).
It has been reported that suicidal ideation and substance abuse were related to PA in patients with schizophrenia11,17 but we did not find any relationship between suicidality, substance abuse and PA in the present sample. Akvardar et al. demonstrated that the prevalence of substance abuse in patients with schizophrenia in Turkey is low.24 The present findings might arise from cultural and religious characteristics of Turkish patients.
We found that patients with panic symptoms had higher PANSS, HDRS, CGI and ESRS scores. Higher PANSS and CGI scores are related to symptom severity of schizophrenia. According to the cognitive behavioral model, the likelihood of having a PA increases with hypervigilance and hyper arousal as well as with the patient’s tendency to attribute physical symptoms to the presence of an external threat. In patients with schizophrenia, this perceived threat may parallel their positive symptoms; hence they already believe that something bad is going to happen even before they start experiencing the symptoms of PA. The PA then reinforces this belief that something bad is going to happen and thus begins a vicious cycle.10 This vicious cycle may increase the positive and depressive symptoms of schizophrenia patients with PA.
We found that extrapyramidal side-effects were related to panic symptoms in patients with schizophrenia, as previously reported.8 This relationship may be due to the drug regimen but the relationship between drug doses and panic symptoms was not assessed.
Although Bayle et al. did not find significant difference for schizophrenia onset between patients with schizophrenia who suffered from PAand those who did not; we found that panic symptoms were significantly higher in patients with early onset schizophrenia.16 Small sample size was the primary limitation of the present study.There may be a different form of schizophrenia or a subtype of the disorder associated with PA having a worse outcome, but further studies will be needed to confirm this finding.
References
- Kessler RC, McGonagle KA, Zhao S et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 1994; 51: 8–19.
- Katerndahl DA,Realini JP. Lifetime prevalence of panic states. Am. J. Psychiatry 1993; 150: 246–249.
- Eaton WW, Kessler RC, Wittchen HU et al. Panic and panic disorder in the United States. Am. J. Psychiatry 1994; 151: 413–420.
- Regier DA, Kaelber CT, Rae DS et al. Limitations of diagnostic instruments for mental disorders: Implications for research and policy. Arch. Gen. Psychiatry 1998; 55: 109–115.
- Weissman MM, Bland RC, Canino GJ et al. The crossnational epidemiology of panic disorder. Arch.Gen. Psychiatry 1997; 54: 305–309.
- Kessler RC, Chiu WT, Jin R et al. The epidemiology of panic attacks, panic disorder, and agoraphobia in the national comorbidity survey replication. Arch. Gen. Psychiatry 2006; 63: 415–424.
- Pitch RJ, Bermanzohn PC, Siris SG. Panic symptoms in patients with schizophrenia. In: Hwang MY, Bemanzohn PC (eds). Schizophrenia and Comorbid Conditions. American Psychiatric Press, Washington, DC; 2001; 79–95.
- Higuchi H, Kamata M, Yoshimoto M, Shimisu T, Hishikawa Y. Panic attacks in patients with chronic schizophrenia: A complication of long-term neuroleptic treatment. Psychiatry Clin. Neurosci. 1999; 53: 91–94.
- Argyle N. Panic Attacks in chronic schizophrenia. Br. J. Psychiatry 1990; 157: 430–433.
- Labbate LA, Young PC, Arana GW. Panic disorder in schizophrenia. Can. J. Psychiatry 1999; 44: 488–490.
- Goodwin R, Lyons JS, McNally RJ. Panic attacks in schizophrenia. Schizophr. Res. 2002; 58: 213–220.
- Weissman MM, Klerman GL, Markowitz JS et al. Suicidal ideation and suicide attempts in panic disorder and attacks. N. Engl. J. Med. 1989; 18: 1209–1214.
- Bermanzohn PC, Arlow PB, Pollack S et al. At issue: Hierarchical diagnosis in chronic schizophrenia: A clinical study of co-occurring syndromes. Schizophr. Bull. 2000; 26: 517–525.
- Kessler RC. The prevalence of psychiatric comorbidity. In: Wetzler S, Sanderson WC (eds). Treatment Strategies for Patients with Psychiatric Comorbidity. John Wiley & Sons, New York, 1997; 23–48.
- Goodwin G, Stayner DA, Chinman MJ et al. Impact of panic attacks on rehabilitation and quality of life among persons with severe psychotic disorders. Psychiatr. Serv. 2001; 52: 920–924.
- Bayle FJ, Krebs MO, Epelbaum C, Levy D, Hardy P. Clinical features of panic attacks in schizophrenia. Eur. Psychiatry 2001; 16: 349–353.
- Goodwin R, Davidson L. Panic attacks in psychosis. Acta Psychiatr. Scand. 2002; 105: 14–19.
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Clinical Version (SCID-I/CV). American Psychiatric Press, Washington, DC, 1997.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987; 13: 399–404.
- Williams BW.A structured interview guide for Hamilton Depression Rating Scale. Arch. Gen. Psychiatry 1978; 45: 742–747.
- GuyW.ECDEU:Assessment Manual for Psychopharmacology, US Department Health Education and Welfare publication (ADM) 76-338. National Institute of Mental Health, Rockville, MD, 1976; 218–222.
- Chouinard G, Ross-Chouinard A, Annable L. Extrapyramidal symptom rating scale. Can. J. Neurol. Sci. 1980; 7: 233.
- Bandelow B. Assessing the efficacy of treatments for panic disorder and agoraphobia II. The Panic and Agoraphobia Scale. Int. Clin. Psychopharmacol. 1995; 10: 73–81.
- Akvardar Y, Tumuklu M, Akdede BB, Ulas H, Kitis A, Alptekin K. Substance use among patients with schizophrenia in a university hospital. Bull. Clin. Psychopharmacol. 2004; 14: 191–197 (in Turkish).
