Effects of quetiapine on cognitive functions in schizophrenia
Effects of quetiapine on cognitive functions in schizophrenia
Berna Binnur Kivircik Akdede*, Koksal Alptekin, Arzu Kitiş, Haluk Arkar, Yildiz Akvardar
Department of Psychiatry, Dokuz Eylu¨ l University School of Medicine, Balc¸ova, InciraltV Izmir, Turkey
Accepted 19 November 2004
Available online 24 December 2004
Abstract
Objective: All atypical antipsychotic drugs with complex pharmacology have been shown to improve some, but not all, domains of cognitive function, including quetiapine, i.e., the agent with the most rapid dissociation from dopamine receptors and a relatively weak serotonin antagonism. The present study was to evaluate which, if any, areas of cognition improve in patients with schizophrenia, following a brief treatment with quetiapine.
Methods: Effects of quetiapine on cognition were investigated in a group of patients with schizophrenia (n=14). Neuropsychological tests in cognitive areas previously shown as impaired in schizophrenia were administered at baseline and after 8 weeks of treatment with quetiapine. Administered at these two times were also the Positive and Negative Syndrome Scale, Hamilton Depression Rating Scale, and scales to assess motor side effects (Abnormal Involuntary Movement Scale, Simpson-Angus Scale, and Barnes Akathisia Scale)..
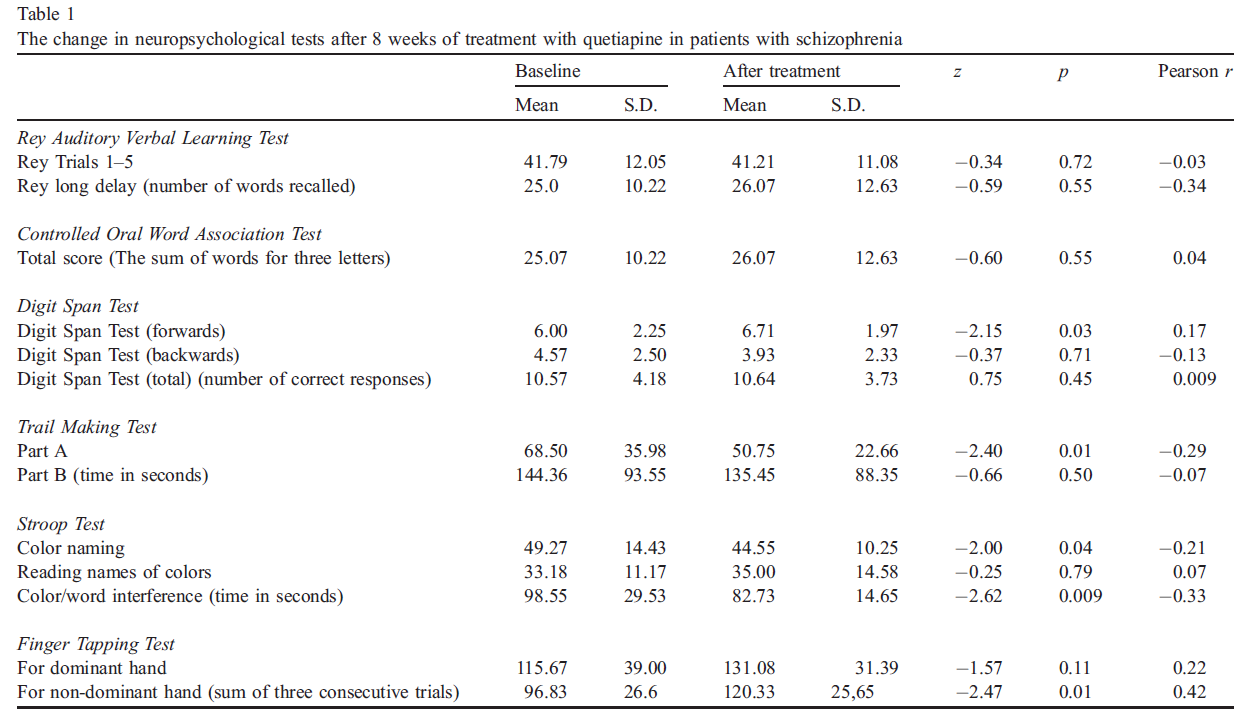
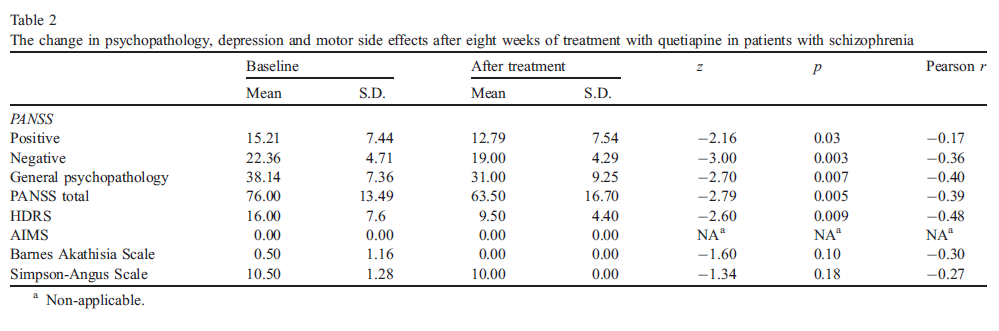
Results: Wilcoxon Signed Ranks Test indicated a statistically significant improvement in scores on Digit Span Test, Trail Making Test, Stroop Test, Finger Tapping Test, and on the Positive and Negative Syndrome Scale. No significant change was noted in motor side effects.
Conclusion: The patients improved in their attentional, motor, and visuo-motor skills, and in executive functions as well as with respect to psychopathology, without an increase in motor side effects.
© 2004 Elsevier Inc. All rights reserved.
Keywords: Cognitive function; Quetiapine; Schizophrenia
Abbreviations: AIMS, Abnormal Involuntary Movement Scale; HDRS, Hamilton Depression Rating Scale; PANSS, Positive and Negative Syndrome Scale.
* Corresponding author. Tel.: +90 232 4124158 fax: +90 232 2782366
* E-mail adress:[email protected] (B.B. Kivircik Akdede).
0278-5846/$ - see front matter © 2004 Elsevier Inc. All rights reserved. doi:10.1016/j.pnpbp.2004.11.005
1.Introduction
Impairments in neurocognitive functioning along with positive and negative symptoms are a characteristic of most patients with schizophrenia. Widespread impairments were documented in numerous domains of neurocognitive functioning, including the executive functions, attentional skills, perceptual and motor processing, vigilance, verbal learning and memory, spatial working memory, and verbal fluency (Braff et al., 1991; Kenny and Meltzer, 1991; Saykin et al.,1994). Recent investigations have demonstrated generalized cognitive deficits also in patients with first episode schizophrenia (Mohamed et al., 1999; Bilder et al., 2000).However, in contrast to reports of a generalized cognitive dysfunction, some studies suggest a more selective cognitive dysfunction (Saykin et al., 1991). In general, the researchers agree that not all domains of cognition are equally impaired in individual patients with schizophrenia.
Level of cognitive functioning has increasingly been regarded as a crucial dimension of in the assessment of treatment outcomes in schizophrenia. In fact, the neurocognitive deficits appear predictive of social functioning, occupational functioning and the capacity for of independent living in the community (Green, 1996; Velligan and Miller, 1999; Meltzer et al., 1996).
All atypical antipsychotics with complex pharmacology, including clozapine, olanzapine, quetiapine, risperidone and ziprasidone have been observed to improve some, but not all, aspects of cognitive functioning such as perceptual and motor processing, attention, executive functions, verbal learning, verbal memory, and working memory (Hagger et al., 1993; Hoff et al., 1996; Green et al., 1997; Purdon et al., 2000; Weickert et al., 2003). Major beneficial effects of both clozapine and olanzapine have been noted with respect to verbal fluency (Meltzer and McGurk, 1999). Risperidone has been found to have a beneficial effect on working memory (Green et al., 1997). Different atypical agents may tackle different aspects of cognitive function in schizophrenia.
Studies comparing the effects of different atypical agents on cognition have led to somewhat inconsistent results. For example, while a comparison, by Purdon et al. (2000), of olanzapine, risperidone and haloperidol suggested a superiority of olanzapine over risperidone, Harvey’s (2000) study on a larger sample size showed no significant difference. A more recent comparison of the neurocognitive impact of clozapine, olanzapine, risperidone and haloperidol showed an overall superiority of olanzapine and risperidone over haloperidol, however, olanzapine and risperidone did not significantly differ from each other and from clozapine in terms of global cognitive performance (Bilder et al., 2002).
As the pharmacological profile of quetiapine differs from clozapine, olanzapine and risperidone with respect to certain serotonergic, dopaminergic and adrenergic receptors, the effects of quetiapine on cognition might differ from those of the other atypical antipsychotics. Quetiapine has a higher affinity for 5-HT2 than dopamine D2 receptors, but unlike clozapine it shows minimal intrinsic anticholinergic activities (Saller and Salama, 1993). Both quetiapine and clozapine dissociate much more rapidly from dopamine D2 receptors than other atypicals which differ relatively little from typical neuroleptics in this respect (Seeman and Tallerico, 1999).
An open label study investigating cognitive effects of quetiapine in schizophrenia reported improvement in attention (Sax et al., 1998). Later on, two double-blind comparisons of cognitive effects of quetiapine and haloperidol demonstrated significant improvements in verbal reasoning, verbal fluency, executive functions, and verbal memory in chronically ill schizophrenic patients (Velligan et al., 2002; Purdon et al., 2001). Another recent study has reported significant improvements in attention, verbal fluency and executive function after quetiapine treatment of patients with first episode of schizophrenia and related disorders (Good et al., 2002).
The goal of the present study was to evaluate which, if any, areas of cognition improve in patients with schizophrenia, following a brief treatment with quetiapine.
2.Methods
2.1. Patient sample
Eighteen patients who met DSM-IV (American Psychiatric Association, 1994) criteria for schizophrenia were accepted for the study. All of these had no history of a serious medical disease or of neurological disorders, were considered free of recent substance abuse, and received no electroconvulsive therapy in the last 6 months. All patients gave a written informed consent. All except two patients were followed up in an outpatient clinic. Four patients withdrew from the study: two of them reportedly due to lack of effect and the other two had reconsidered and withdrew their consent. Our statistical analysis was carried out on the data of the remaining 14 patients (4 women and 10 men).
Their mean age was 32.3 years (S.D.=9.8), their mean level of education was 10.0 years (S.D.=3.1), and the mean duration of their mental disease was 8.2 years (S.D.=6.1). Prior to our quetiapine study, 9 were taking atypical antipsychotics (2 patients were on clozapine, three on risperidone, and 4 on olanzapine), 3 patients were on typical antipsychotics (2 on haloperidol and 1 on pimozid), and 2 of the 14 patients were drug-free.
2.2. Drug administration
The patients were administered 50 mg/day of quetiapine on the first day, 100 mg/day on the second, 200 mg/day on the third and 300 mg/day on the fourth day. Taking into account their response, the dose was raised to 400–700 mg/ day. The drug was given twice per day. The mean dose was 478.5 mg/day (S.D.=167.2).
All patients had a washout period of 2 to 7 days. Patients receiving depot antipsychotic drugs within the last month were not included in our study. Our patients were allowed to take benzodiazepines throughout the washout period, with the exception of the day before baseline testing. They used benzodiazepines only as a concurrent medication (with quetiapine) during the subsequent study period.
2.3. Assessment instruments
A series of neuropsychological tests was administered at baseline and repeated after 8 weeks of treatment. The tests measured 5 key factors that are frequently impaired in patients with schizophrenia. The first of these factors involves verbal learning and memory and was assessed in our study via Rey Auditory Verbal Learning Test. This test consists of five presentations and a recall of a 15 word list, one presentation of a second 15 word list, and a sixth recall trial. The patient’s score on each trial consists of the number of correctly recalled words. A total score, i.e., the sum of trials 1 through 5, is calculated. The number of words recalled after 20 to 30 min provides the delayed recall score (Lezak, 1995).
The second key factor assessed in this study is verbal fluency and was assessed via Controlled Oral Word Association Test. This test evaluates spontaneous production of words beginning with a given letter within a brief amount of time. The letters F, A, and S are the most commonly used in this test. However, the letters K, A, S were used in the present study due to their relative frequency in Turkish. The patient’s score is the sum of all admissible words for these three letters (Spreen and Strauss, 1998).
The third key factor involves attentional skills and was evaluated via the Digit Span Test, as published in the Wechsler batteries (Wechsler, 1987). It is commonly used to quantify immediate verbal recall (Lezak, 1995). In the first section of this test (known as Digits Forward), the patient repeats series of digits read to him or her by the examiner. In the second section of this test (known as Digits Backward), the patient has to reverse the order of the series of digits. The scores consist of the sum of correctly recalled series of numbers on each of the two sections separately as well as the sum of these two subscores.
The fourth key factor assessed in this study involves executive skills and visuo-motor tracking and has been measured by the Trail Making Test. This is a timed test that evaluates attention, sequencing skills, and mental flexibility as well as the visual search skills and motor functioning (Spreen and Strauss, 1998). In the part A of this test, the patient is asked to connect, in a correct ascending sequence, with a continuous line the digits ranging from 1 to 25, dispersed on a preprinted standard sheet of paper. In the part B, the patient is asked to alternate connecting digits (in an ascending order) and letters (in alphabetical order). As this part (part B) is closely correlated with tests of timed executive functioning, it is now often interpreted in neuropsychology as a measure of executive skills (Libon et al., 1994). The measures include the time (in seconds) to complete each part of the test.
We have also administered the Stroop Test to measure the ease with which the patient can shift his or her perceptual set to adapt to the changing nature of tasks and suppress a habitual response in favor of a novel approach, as an aspect of executive functioning (Spreen and Strauss, 1998). It involves naming of colors, reading of printed names of colors, and a color/word interference condition. The score is the time needed to complete the various sections of this test.
The fifth neuropsychological key factor assessed in this study is motor skills and these were measured via the Finger Tapping Test. It evaluates the motor speed of the index finger of each hand (Spreen and Strauss, 1998). The score is usually computed for each hand separately and consists of the mean of five consecutive 10-s trials. In the present study, we recorded the sum of 3 consecutive trials.
We administered the following rating scales for psychopathology and motor side effects both at baseline and after 8 weeks on quetiapine. To rate the severity of the psychotic illness, we used the Positive and Negative Syndrome Scale (PANSS, see Kay et al., 1987) in its Turkish edition (Kostakoglu et al., 1999). The Hamilton Depression Rating Scale (HDRS, see Williamss, 1978; for Turkish edition, see Akdemir et al., 1996) was used to rate depressive symptoms. The motor side effects were assessed via Abnormal Involuntary Movement Scale (AIMS) described in Guy (1976), Simpson-Angus Scale (Simpson and Angus, 1970) and Barnes Akathisia Scale (Barnes, 1989).
2.4. Statistical analysis
The changes in neuropsychological test scores over time as well as the changes in scores on the PANSS, HDRS, AIMS, Simpson-Angus Scale, and on the Barnes Akathisia Scale were evaluated with the Wilcoxon Signed Rank Test.
Pearson (point biserial) correlation test was conducted to indicate the magnitude of the changes on all variables conceptualizing the pretest versus post-test as a dichotomy.
Pearson correlation test was also used to investigate the relationships between the change on PANSS scores (pretest minus post-test) and the amount of change on neuropsychological test scores (pretest minus post-test). The correlations between the change on neuropsychological test scores and the amount of change on AIMS, Barnes Akathisia Scale, and Simpson-Angus Scale scores were analyzed with Pearson correlation test, as well.
3.Results
3.1. The effects of quetiapine on cognition
A statistically significant improvement was found on four neuropsychological tests: the Trail Making Test, Stroop Test, Digit Span, and the Finger Tapping Test (see Table 1). Specifically, our patients improved over the 8 weeks of quetiapine treatment on the part A of Trail Making Test and on the Digits Forward section of Digit Span Test. The patients also obtained better scores in the color naming and color/word interference condition of the Stroop Test. The improvement on the Finger Tapping Test was significant only for the non-dominant hand. The Pearson (point biserial) correlation coefficients for all neuropsychological test scores were shown in Table 1.
3.2. The effects of quetiapine on psychopathology and motor side effects
PANSS total scores and HDRS scores decreased significantly ( pb0.01) over time (Table 2). Our patients have significantly improved on all three subscales of the PANSS, i.e., on the positive ( pb0.05), the negative ( pb0.01), and the general ( pb0.01) subscales. There was no significant change in AIMS, Barnes Akathisia Scale, and Simpson-Angus Scale over time and this indicates no overall motor side effects with quetiapine ( pN0.05). The Pearson (point biserial) correlation coefficients for all these variables were shown in Table 2.
3.3. Correlations between the change on PANSS scores and the amount of change on neuropsychological test scores
The change on PANSS total scores was correlated only with the change on Rey Auditory Verbal Learning Test delayed recall scores ( p=0.01, r=-0.64) and Digit Span Test total scores ( p=0.001, r=-0.78).
3.4. Correlations between the change on neuropsychological test scores and the amount of change on AIMS, Barnes Akathisia Scale, and Simpson-Angus Scale scores
The change on neuropsychological tests was not correlated to the amount of change on the scores of the tests rating motor side effects.
4. Discussion
The main finding in our study indicates that the 8-week treatment via quetiapine has produced a significant improvement in attentional, visuo-motor and motor skills, executive functioning, and also resulted in a decrease in the level of psychopathology. The improvement in cognitive parameters appears to be independent of the improvement in psychopathology, except attention. No significant improvement in secondary memory or semantic memory functioning was noted.
4.1. The effects of quetiapine on cognition
Our results are partially consistent with other open label studies and also with previous controlled studies that investigated the effects of quetiapine on cognition and found a significant improvement, both in short- and in a long-term treatments (Sax et al., 1998; Fleming et al., 2001, Purdon et al., 2001; Velligan et al., 2002, 2003).
Sax et al. (1998) observed a marked improvement associated with quetiapine treatment, with respect to attentional skills: after 2 months, their small group (n=10) of patients with schizophrenia no longer significantly differed from that of a matched control group. Fleming et al. (2001) have reported a significant improvement in attentional skills as well as a trend towards an improvement on tests of motor speed and of set shifting (Trail Test, part B) and of verbal fluency in a small sample of subjects with various diagnoses following a brief trial.
Executive functioning as measured by the interference part of Stroop test in our study and as measured by part B of Trail Making Test in the study by Fleming et al. (2001) appears to be improved by quetiapine. While the neuropsychological tests varied from study to study, the improvement in attentional, motor, and executive functioning was noteworthy and similar to our study.
With respect to randomized controlled studies, both a 6-month-long study by Purdon et al. (2001) and a 24-weekstudy by Velligan et al. (2002) comparing the effects of quetiapine with those of haloperidol on cognition reported a significant improvement with quetiapine, in particular on tests of verbal reasoning and fluency, verbal memory, executive skills, and visuospatial construction, and verbal fluency. In our relatively brief study (only 8 weeks), no significant improvement was noted on tests of verbal fluency and memory but the patients significantly improved on visuo-motor tracking and executive functions.
4.2. Relation of the improvement in cognitive functions to psychopathology
Although the small size of our sample and the brief duration of the trial in the present study preclude extensive generalizations, it appears that the performance on neuropsychological tests after quetiapine treatment is independent on the improvement in psychopathology, except attention. As a measure of attention, the change on Digit Span Test showed a significant high correlation to the change on total scores of PANSS. The recent investigation by Velligan et al. (2002) has also suggested that the improvement in cognitive tests was not due to changes in psychopathology. Since quetiapine has also been found to improve cognitive parameters in first episodic psychotic patients, this indicates that quetiapine’s effect on cognition is not in some manner due to chronicity of the illness or psychopathology (Good et al., 2002).
The improvements induced by quetiapine in attention and executive functions have been reported in various studies based on different designs, including our study. With respect to other atypical antipsychotics, improvements on measures of verbal memory and fluency with clozapine and olanzapine and the improvement of verbal working memory with risperidone suggest that these might be the specific major neurocognitive areas that improve with these particular pharmacological agents (Meltzer and McGurk, 1999; Green et al., 1997). While quetiapine has also been reported to improve verbal memory and fluency in some of the studies (Purdon et al., 2001; Velligan et al., 2002), we have not been able to confirm this in our study. However, our present study may have perhaps been relatively too brief to allow for the improvement to manifest on these particular cognitive parameters. Further investigations comparing quetiapine with other atypical drugs would hopefully provide more long-term data.
The main limitation of our study was the small sample size. Pearson (point biserial) correlation analysis showed that the magnitude of the change on neuropsychological tests was quite small. Other limitations of our study include a relatively high drop-out ratio, a lack of a matched control group, the brief duration, and the open label design. These factors restrict the generalization of our findings. Furthermore, our washout period may have been too short to prevent confounding effects of prior antipsychotic drugs on our baseline neuropsychological evaluations. More extensive investigations of long-term neuropsychological effects of quetiapine are needed.
5. Conclusion
The present study suggests that quetiapine improves specific areas of neurocognitive function and suppresses positive and negative symptoms of schizophrenia, without an increase in motor side effects.
Acknowledgment
The present study was presented in a poster session at the International Congress on Schizophrenia Research in 2003.
References
- Akdemir, A., O¨ rsel, S., DaW, Y´., Tqrkc¸apar, H., I˙Yc¸an, N., O¨ zbay, H., 1996. Validity, reliability and clinical utilization of Hamilton depression rating scale. J. Psychiatry Psychol. Psychopharmacol. 4, 251–259.
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC.
- Barnes, T.R.E., 1989. A rating scale for drug induced akathisia. Br. J. Psychiatry 1564, 672–676.
- Bilder, R.M., Goldman, R.S., Robinson, D., Reiter, G., Bell, L., Bates, J., Pappadopulos, E., Wilson, D.F., Alvir, J.M.J., Woerner, M., Geisler, S., Kane, J., Lieberman, J.A., 2000. Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am. J. Psychiatry 157, 549–559.
- Bilder, R.M., Goldman, R.S., Volavka, J., Czobor, P., Hoptman, M., Sheitman, B., Lindenmayer, J.P., Citrome, L., McEvoy, J., Kunz, M., Chakos, M., Cooper, T.B., Horowitz, T.L., Lieberman, J.A., 2002. Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperidol in patients with chronic schizophrenia or schizoaffective disorder. Am. J. Psychiatry 159, 1018– 1028.
- Braff, D.L., Heaton, R., Kuck, J., Cullum, M., Moranville, J., Grant, I., Zisook, S., 1991. The generalized pattern of neuropsychological deficits in outpatients with chronic schizophrenia with heterogeneous Wisconsin card sorting test results. Arch. Gen. Psychiatry 48, 891–898.
- Fleming, K., Thyrum, P., Yeh, C., Vargo, D., Potkin, S., 2001. Cognitive improvements in psychotic subjects treated with bseroquelQ (quetiapine fumarate): an exploratory study. J. Clin. Psychopharmacol. 21, 527– 529.
- Good, K.P., Kiss, I., Buiteman, C., Woodley, H., Rui, Q., Whitehorn, D., Kopala, L., 2002. Improvement in cognitive functioning in patients with first-episode psychosis during treatment with quetiapine: an interim analysis. Br. J. Psychiatry 43, 45– 49.
- Green, M.F., 1996. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry 153, 321– 330.
- Green, M.F., Marshall, B.D., Wirshing, W.C., Ames, D., Marder, S.R., McGurk, S.R., Kern, R.S., Mintz, J., 1997. Does risperidone improve verbal working memory in schizophrenia? Am. J. Psychiatry 154, 799– 804.
- Guy, W., 1976. Abnormal Involuntary Movement Scale (AIMS) ECDEU Assessment Manual for Psychopharmacology, Revised. National Institute of Mental Health, Department of Health, Education and Welfare. Rockville (MD), pp. 78– 388.
- Hagger, C., Buckley, P., Kenny, J.T., Friedman, L., Ubogy, D., Meltzer, H.Y., 1993. Improvement in cognitive functions and psychiatricsymptoms in treatment refractory schizophrenic patients receiving clozapine. Biol. Psychiatry 34, 702– 712.
- Harvey, P.D., 2000. Cognitive effects of risperidone and olanzapine in patients with schizophrenia or schizoaffective disorder. 2000 Annual Meeting New Research Programme and Abstracts. American Psychiatric Association, Washington, DC, p. 149.
- Hoff, A.L., Faustman, W.O., Wieneke, M., Espinoza, S., Costa, M., Wolkowitz, O., Csernansky, J.C., 1996. The effects of clozapine on symptom reduction, neurocognitive function, and clinical management in treatment refractory state hospital schizophrenic inpatients. Am. J. Psychiatry 149, 898–903.
- Kay, S.R., Fiszbein, A., Opler, L.A., 1987. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261– 276.
- Kenny, J.T., Meltzer, H.Y., 1991. Attention and higher cortical functions in schizophrenia. J. Neuropsychiatry 3, 269– 275.
- Kostakoglu, A.E., Batur, S., Tiryaki, A., 1999. The validity and reliability of the Turkish version of the Positive and Negative Syndrome Scale (PANSS). Turk. J. Psychol. 14, 23–32.
- Lezak, M.D., 1995. Neuropsychological assessment, third. ed. Oxford University Press, New York.
- Libon, D.J., Glosser, G., Malamut, B.L., Kaplan, E., Goldberg, E., Swenson, R., Sands, L.P., 1994. Age, executive functions, and visuospatial functioning in healthy older adults. Neuropsychology 8, 38– 43.
- Meltzer, H.Y., McGurk, S.R., 1999. The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr. Bull. 25, 233– 255.
- Meltzer, H.Y., Thompson, P.A., Lee, M.A., Ranjan, R., 1996. Neuropsychological deficits in schizophrenia: relation to social function and effect of antipsychotic drug treatment. Neuropsychopharmacology 14, 27S–33S.
- Mohamed, S., Paulsen, J.S., O’Leary, D., Arndt, S., Andreasen, N., 1999. Generalized cognitive deficits in schizophrenia: a study of first-episode patients. Arch. Gen. Psychiatry 56, 749–754.
- Purdon, S.E., Jones, B.D., Stip, E., Labella, A., Addington, D., David, S.R., Breier, A., Tollefson, G.D., 2000. Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. Arch. Gen. Psychiatry 57, 249– 258.
- Purdon, S.E., Malla, A., Labella, A., Lit, W., 2001. Neuropsychological change in patients with schizophrenia after treatment with quetiapine or haloperidol. J. Psychiatry Neurosci. 26, 137–149.
- Saller, C.F., Salama, A.I., 1993. Seroquel: biochemical profile of a potential atypical antipsychotic. Psychopharmacology 112, 285–292.
- Sax, K.W., Strakowski, S.M., Keck, P.E., 1998. Attentional improvement following quetiapine fumarate treatment in schizophrenia. Schizophr. Res. 33, 151– 155.
- Saykin, A.J., Gur, R.C., Gur, R.E., Mozley, P.D., Mozley, L.H., Resnick, S.M., Kester, B., Stafiniak, P., 1991. Neuropsychological function in schizophrenia: selective impairment in memory and learning. Arch. Gen. Psychiatry 48, 618–624.
- Saykin, A.J., Shtasel, D.L., Gur, R.E., Kester, D.B., Mozley, L.H., Stafiniak, P., Gur, R.C., 1994. Neuropsychological deficits in neuroleptic naive patients with first episode schizophrenia. Arch. Gen. Psychiatry 51, 124–131.
- Seeman, P., Tallerico, T., 1999. Rapid release of antipsychotic drugs from dopamine D2 receptors: an explanation for low receptor occupancy and early clinical relapse upon withdrawal of clozapine and quetiapine. Am. J. Psychiatry 156, 876–884.
- Simpson, G.M., Angus, J.W.S., 1970. A rating scale for extra-pyramidal side effects. Acta Psychiatr. Scand. 212, 44– 51.
- Spreen, O., Strauss, E., 1998. A compendium of neuropsychological tests: administration, norms, and commentary, second ed. Oxford University Press, New York.
- Velligan, D.I., Miller, A.L., 1999. Cognitive dysfunction in schizophrenia and its importance to outcome: the place of atypical antipsychotics in treatment. J. Clin. Psychiatry 60 (Suppl. 23), S25–S28.
- Velligan, D.I., Newcomer, J., Pultz, J., Csernansky, J., Hoff, A.L., Mahurin, R., Miller, A.L., 2002. Does cognitive function improve with quetiapine in comparison to haloperidol? Schizophr. Res. 53, 239–248.
- Velligan, D.I., Prihoda, T.J., Sui, D., Ritch, J.L., Miller, A.L., 2003. The effectiveness of quetiapine versus conventional antipsychotics in improving cognitive and functional outcomes in standard treatment settings. J. Clin. Psychiatry 64, 524– 531.
- Wechsler, D., 1987. Wechsler Memory Scale-Revised. The Pychological Corporation, San Antonio, TX.
- Weickert, T.W., Goldberg, T.E., Marenco, S., Bigelow, L.B., Egan, M.F., Weiberger, D.R., 2003. Comparison of cognitive performances during a placebo period and an atypical antipsychotic treatment period in schizophrenia: critical examination of confounds. Neuropsychopharmacology 28, 1491– 1500.
- Williamss, B.W., 1978. A structured interview guide for Hamilton depression scale. Arch. Gen. Psychiatry 45, 742– 747.
